Using chemotherapy to fight malaria

The battle to conquer the deadly malaria parasite could soon take an unexpected turn as University of Melbourne researchers bring chemotherapy drugs into the armoury.
Leading malaria researcher Professor Leann Tilley and her team have uncovered the mechanism of how frontline antimalarial drug, artemisinin, works and are now working on a promising chemotherapy-based compound to treat patients.

Artemisinin is derived from wormwood and was developed in China during Mao Zedong’s rule. It has saved millions of lives, but scientists are engaged in a constant game of cat-and-mouse with malaria, searching for ways to beat the parasite’s growing resistance.
Malaria claims the lives of about 440,000 people worldwide every year, the majority of whom are children under five years of age, and artemisinin resistance has developed in South-East Asia, with fears it will soon reach Africa.
Exposing malaria's atomic machinery
“If you’re going into a coma suffering very serious complications from malaria, you need immediate relief from the symptoms and this drug works very quickly,” Professor Tilley says.
But there are at least two catches.
First, artemisinin doesn’t work very well by itself. It effectively reduces the parasite’s impact, but doesn’t kill off every parasite infecting an individual.
Hence artemisinin is always used in combination with other antimalarial drugs.
But here comes the second catch; resistance is rising to both artemisinin and the partner drugs.
“The combination of artemisinin and various partner drugs reduces the patient’s symptoms and stops them from dying, but no longer cures them. A few weeks later malaria comes back and the patient has to return for more treatment; but doctors are running out of treatment options.”
Clearly there’s a degree of urgency.

“Although we have very good scientists working on malaria, and we are making progress, there’s a risk that we could go backwards very quickly if resistance spreads to Africa,” she says.
Understanding artemisinin
It’s surprisingly common not to know exactly how and why a drug works. For example, the modes of action of paracetamol, which is used to treat pain, and lithium compounds, which are used to treat bipolar disorder, are not clear.
The genes that turn malaria into a killer
But not knowing how artemisinin works has been a block to understanding the growing resistance and to developing better treatments. Understanding the mechanism underpinning the drug’s action has become mission critical for malaria researchers.
“What we have discovered is that artemisinin packs a double whammy,” says Professor Tilley.
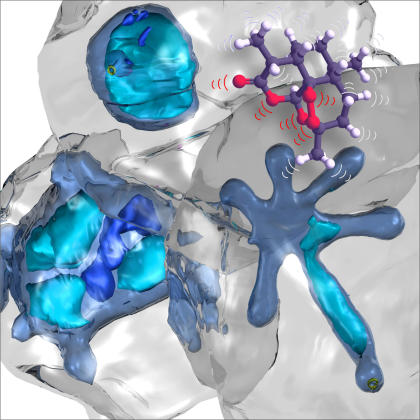
“When it gets inside the malaria parasite it goes off like a cluster bomb, damaging proteins.
“After the ‘explosion’, the parasite is desperately reliant on shredder enzymes, called proteasomes, to dispose of the excess waste. Artemisinin also targets this waste disposal system, further weakening the parasite”
Blockage of the proteasome causes an accumulation of proteins that are marked with a ‘kiss of death’ modification. When these damaged proteins build up, they stress the parasite and soon lead to cell death.
Professor Tilley believes the parasite is becoming resistant to artemisinin by better shielding itself from the cluster bomb.
Enter chemotherapy
Here’s where chemotherapy comes in, because some cancer drugs are designed to attack proteasomes. They are called proteasome inhibitors.
Professor Tilley explains that cancer cells grow at a gangbusters’ rate, creating so much waste they are more reliant on their proteasomes than regular cells.
Hitting cancer cells with proteasome inhibitors kills them.
Working on a hunch, Professor Tilley tried hitting malaria parasites with proteasome inhibitors.
The team discovered that artemisinin and the anti-cancer drugs can work together to knock out the proteasome and prevent the parasite’s ‘shielding’ response.
The results are promising, and have led to Professor Tilley teaming up with Takeda of Japan and Swiss-based non-profit research foundation Medicines for Malaria Venture to discover a new parasite-specific proteasome inhibitor that works in tandem with artemisinin, and advance it to clinical trials.
Malaria patients are already debilitated by the disease, so currently-used chemotherapy drugs could prove too toxic for them.
That’s why Professor Tilley says the new modified drugs will have to only attack the malaria parasite’s proteasome, and not the patient’s.
“We want a compound that can be administered orally and will last a long time in the blood stream.
“If a suitable compound can be found, human trials could happen very soon,” Professor Tilley says.
The new battlefront in malaria research
And Medicines for Malaria Venture can shepherd promising antimalarial compounds through the pipeline from discovery to trial via a fast-tracked approvals process.
After 20 years researching malaria, Professor Tilley has seen great changes in her field, which she was originally drawn to because she wanted her work to make a difference.
“Back when I started, 4 million people a year died of malaria. Now that figure is 450,000. That’s still a lot, but we are making progress,” she says.
Sadly though, with all she has learned about this killer disease, Professor Tilley knows one thing for sure: developing a proteasome inhibitor antimalarial compound won’t solve the problem permanently.
“It’s inevitable that malaria will build resistance to the compound. You have to plan for the fact that resistance will develop.”
Banner image: UNICEF Ethiopia/Flickr
“This article was first published on Pursuit. Read the original article.”




