Teaming up to fight Motor Neurone disease

Read about the trail taking place for the compound Cu(ATSM) in the Sydney Morning Herald, 26 May 2018, by Greg Callaghan
When a person is diagnosed with Motor Neurone Disease (MND), it’s a race against time.
Symptoms are severe: muscle weakness, cramps, slurred speech, weak grip, fatigue, pain, insomnia, behaviour changes and a constant dry mouth.
Many sufferers do not survive past the first five years because the progressive destruction of their brain’s neurons that control muscles means lung failure is inevitable.
There is no cure.
The lack of an effective treatment haunts sufferers, but now, following ten years of work by researchers from the University of Melbourne, Bio21 Molecular Science and Biotechnology Institute and the Florey Institute of Neuroscience and Mental Health, a human trial for a drug that could fight this devastating disease has begun.
This high-stakes research to create a treatment for such an unforgiving disease is a story of true translational science, and collaboration between three scientists, Associate Professors Kevin Barnham, Anthony White and Paul Donnelly, has been the driving force behind this discovery.
“You can’t force collaboration. It’s about rapport; give and take; feedback based on trust,” says Associate Professor Paul Donnelly, from the School of Chemistry and Bio21 Institute, University of Melbourne.
“We’ve shared ideas, resources, chemicals and compounds,” says Paul.
“We’ve shared ideas, resources, chemicals and compounds,” says Paul.
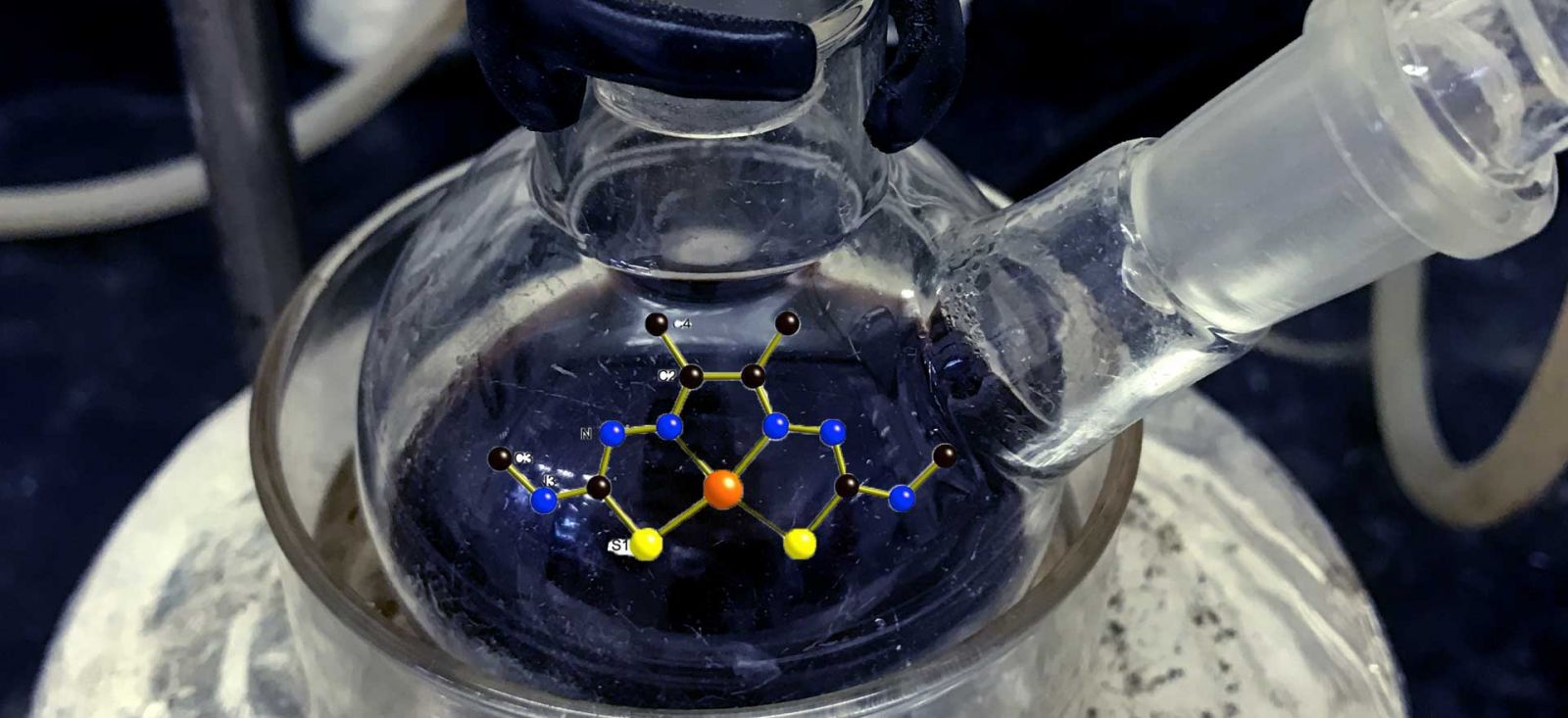
Cu(-ATSM), the trio’s drug to treat motor neuron disease, entered phase I clinical trials at Sydney’s Macquarie University in November.
But before it could reach human trials –– there was years of hard work, with dashes of inspiration and serendipity. Kevin and Paul, whose labs are located on the same floor of the Bio21 Institute, are sitting in my office and I am about to hear their fascinating tale of the potent chemistry of collaboration and copper.
"The initial focus of our work was on Alzheimer's disease where it was thought that copper drove the formation of amyloid plaques. We reasoned if you could just remove this copper you could eliminate plaques, and you’d have the solution,” explains Kevin and so research focused on reducing plaques.
“Then we thought, perhaps it’s the other way around? Maybe cells are expelling the copper and so we’ve actually got a situation of copper deficiency. So, what happens if you deliver the copper back?” Kevin says.
What was needed was a way of delivering copper back into the brain cells. Serendipitously, this is when Kevin was introduced to Paul, who happened to be already working on such molecules.
“I had made 35 different copper compounds which I gave to Kevin and Tony to test,” says Paul.
"This man has a love for chemistry; I’ve never met someone who loves his chemistry this much,” interjects Kevin, pointing at Paul with a laugh.
"This man has a love for chemistry; I’ve never met someone who loves his chemistry this much,” interjects Kevin, pointing at Paul with a laugh.
For Alzheimer’s disease, the compound was Cu(-GTSM); as it is stable in biological systems, cell permeable; it can cross the blood-brain barrier and then it releases copper.
“This gave us the perfect way to test the effect of copper, because we had a perfect control in Cu(-ATSM) that, under normal conditions, does not deliver copper,” explains Kevin. Equipped with the two compounds Cu(-GTSM) and Cu(-ATSM), Kevin and his team began conducting their experiments.
“These have been among the most satisfying experiments I’ve ever done,’ says Kevin.
“These have been among the most satisfying experiments I’ve ever done,’ says Kevin.
“At this time, Tony White and I were part of a NHMRC program grant team, and this flexible funding allowed us to take a few risks and try things that we would not otherwise have done.”
“So we took a punt, and one of the things we tried was Cu(-ATSM) in models of both MND and Parkinson’s disease and it worked brilliantly in both models.”
“The compound has neuroprotective properties, which is useful when targeting neurodegenerative diseases; but there are other properties about this compound that we need to learn more about …,” Kevin says.
Many others played major roles in the project including, Peter Crouch (Pathology), who is the driving force behind much of the recent important work in MND.
The seeds of this remarkable collaboration between this group of chemists, neuroscientists and clinicians were sown back in 2004, when Paul was finishing his postdoc at Oxford University and figuring out what to do next. After reading about the work of Melbourne chemist Tony Wedd on metal biology, and Kevin Barnham and Frances Separovic’s work on brain plaques and copper in Alzheimer’s Disease, he decided: “I need to go to Melbourne to work on metallobiology”.
That same year Kevin Barnham and Tony White, who shared an office, were discussing their scientific frustrations at a lack of progress in Alzheimer’s disease.
“This is when Tony Wedd introduced me to Paul,” recalls Kevin.
“Within six months of arriving in Melbourne, Kevin briefed me on his work and MND, and I introduced him to a family of compounds and we haven’t looked back since,” recalls Paul.
After confirming their potential treatment for MND and Parkinson’s Disease achieved spectacular success in preclinical MND models, the group set up a company and went into business with haematologist-oncologist, Craig Rosenfeld, MD (CEO), whose company, Collaborative Medicinal Development Pty Ltd (CMD), licenced the drug’s intellectual property and has made significant investments to test safety, toxicity and to develop good manufacturing processes for the production of the drug. “You need a believer and Craig Rosenfeld got the science - he reads all our papers,” adds Paul.
The clinical trials started this November at Sydney’s Macquarie University with Dominic Rowe as Principal Investigator. Seeing their theories being tested in the clinic is also a big moment for the Melbourne team.
Both patients and researchers are hopeful. However, the issue of funding remains a sticking point for essential future research.
“We are just scratching the surface of the mountain of compounds Paul has developed,” says Tony White.
“We are just scratching the surface of the mountain of compounds Paul has developed,” says Tony White.
“If we have one drug in clinical trials from the first 20, how many more potential clinical drugs exist in Paul’s library of hundreds?”
“The compounds are there, the knowledge to investigate is there, the techniques exist, we just need funds for researchers to do the work.” says Tony White.

